What Does Atopic Dermatitis Actually Look Like when it Needs Treatment
What Does Atopic Dermatitis Actually Look Like when it Needs Treatment
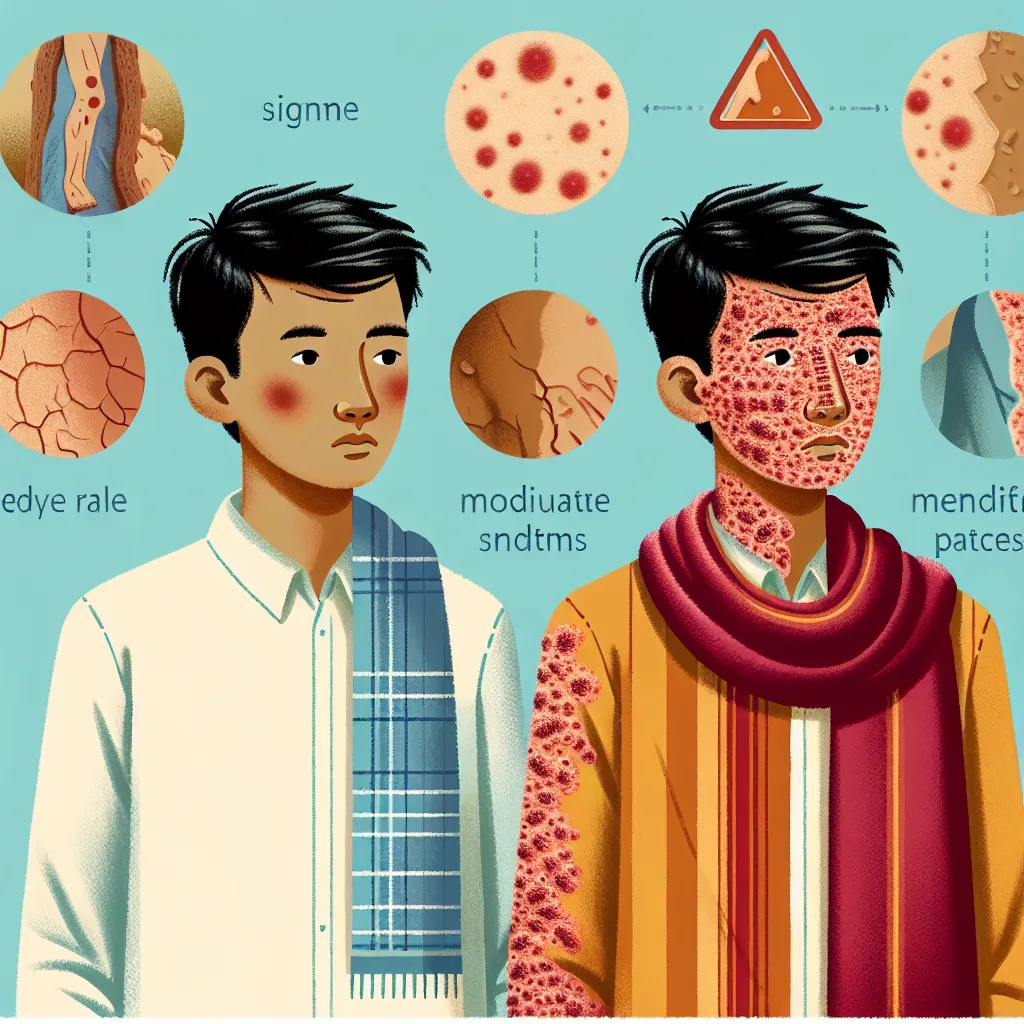
Atopic dermatitis, also known as eczema, is a chronic inflammatory skin condition that affects millions of people worldwide. It is characterized by red, itchy, and inflamed skin, which can be both uncomfortable and distressing for those who experience it. While atopic dermatitis can vary in severity and presentation, it is important to recognize the signs that indicate the need for treatment.
Understanding Atopic Dermatitis
Atopic dermatitis is a multifactorial condition that is influenced by genetic, immunological, and environmental factors. It commonly appears in early childhood but can persist into adulthood or develop later in life. The exact cause of atopic dermatitis is unknown, but it is believed to involve a combination of genetic predisposition, impaired skin barrier function, immune system dysregulation, and environmental triggers.
People with atopic dermatitis often experience periods of flare-ups and remission. During flare-ups, the skin becomes red, dry, itchy, and inflamed. Scratching the affected areas can worsen the symptoms and lead to skin infections. It is crucial to identify the signs that indicate the need for treatment to manage the condition effectively.
Signs That Indicate the Need for Treatment
When atopic dermatitis requires treatment, certain signs become more prominent and may indicate the need for medical intervention. These signs include:
1. Severe Itchiness:
One of the hallmark symptoms of atopic dermatitis is intense itching. Itchiness is often the first indication that the skin condition requires treatment. If the itchiness becomes unbearable and persists despite home remedies and over-the-counter creams, it is important to seek medical advice. Persistent scratching can lead to skin damage and increase the risk of infection.
2. Widespread Rash:
Atopic dermatitis typically starts as red, inflamed patches on the skin. These patches can be local or spread to other areas of the body. If the rash becomes extensive and covers a larger surface area, it may require medical attention. A widespread rash may indicate a more severe flare-up that necessitates prescription treatments to alleviate the symptoms and prevent complications.
3. Skin Infections:
Due to the constant scratching and compromised skin barrier, people with atopic dermatitis are more prone to developing skin infections. Symptoms of infection include increased redness, warmth, swelling, pus-filled blisters, or crusting. If signs of infection are present, medical intervention is crucial to prevent the infection from spreading and to prescribe appropriate antibiotics if necessary.
4. Impact on Daily Life:
If atopic dermatitis starts to affect daily activities, sleep patterns, work, or overall quality of life, it is essential to seek professional help. Chronic itchiness, discomfort, and visible skin lesions can have a significant psychological impact, leading to anxiety, depression, and social withdrawal. Dermatologists can provide appropriate treatment options to reduce symptoms and improve overall well-being.
5. Failure of Home Remedies:
While mild cases of atopic dermatitis can often be managed with over-the-counter creams, moisturizers, and lifestyle adjustments, more severe cases may require prescription medications. If home remedies and non-prescription treatments fail to provide relief or if the condition worsens despite these efforts, it is advisable to consult a dermatologist for a comprehensive evaluation and personalized treatment plan.
Treatment Options for Atopic Dermatitis
When atopic dermatitis requires treatment, several options may be considered based on the severity of the condition and individual patient factors. Common treatment approaches include:
1. Topical Corticosteroids:
Corticosteroid creams or ointments are frequently prescribed to reduce inflammation and relieve itching. They are available in various strengths and are typically applied directly to the affected areas. Long-term use of potent corticosteroids should be monitored by a healthcare professional to minimize side effects.
2. Topical Calcineurin Inhibitors:
Calcineurin inhibitors, such as tacrolimus and pimecrolimus, are non-steroidal medications that suppress the immune response in the skin. They are particularly useful in sensitive areas such as the face and groin, where long-term corticosteroid use may be undesirable.
3. Moisturizers and Emollients:
Regularly applying moisturizers and emollients helps restore the skin barrier, reduce dryness, and prevent flare-ups. These products should be fragrance-free and hypoallergenic to avoid further irritation.
4. Oral Antihistamines:
Antihistamines can help alleviate itching and improve sleep quality. Non-drowsy options are available, but sedating antihistamines may be recommended at night to promote better rest.
5. Systemic Medications:
In severe cases of atopic dermatitis that do not respond to topical treatments, systemic medications may be prescribed. These may include immunosuppressants, oral corticosteroids, or biologic agents that target specific immune pathways involved in the inflammation.
6. Wet Wrap Therapy:
Wet wrap therapy involves applying a moisturizer or topical medication to the affected areas and covering them with wet bandages or clothing. This technique helps hydrate the skin, reduce itching, and enhance the penetration of medications. It should be performed under medical supervision.
Conclusion
Atopic dermatitis, or eczema, can significantly impact the quality of life for those affected. Recognizing the signs that indicate the need for treatment is crucial to effectively manage the condition and prevent complications. Severe itchiness, widespread rash, skin infections, impact on daily life, and failure of home remedies are all indications that medical intervention is necessary. Various treatment options, such as topical corticosteroids, calcineurin inhibitors, moisturizers, antihistamines, systemic medications, and wet wrap therapy, can be used to alleviate symptoms and improve overall well-being. Consulting a dermatologist is recommended for a comprehensive evaluation and personalized treatment plan.
